Residential Care
DIGITAL SOLUTIONS FOR HEALTH CARE

Aspirator Pumps
Rationale (4 line justifying the need of using the solution)
Aspirator Pumps (medical suction machines) are used a wide variety of medical/surgical procedures from everywhere from hospitals, clinics, private practice, EMS, to homecare. Aspirator Pumps help medical staff and users remove body fluids as for example, surgical intervention that involves leakage of blood, mucus, saliva etc. Suction machines are available in portable, tabletop, mobile models. Some smaller, portable units have rechargeable batteries to give users greater mobility.
Professional, clinical aspirators are generally designed for either general or specific applications. These include general use, gastric drainage, thoracic drainage, surgical, uterine and ear, nose and throat (ENT) and dental suction.
Features of the solution (how the solution works)
A suction machine, also known as an aspirator, is a type of medical device that is primarily used for removing obstructions — like mucus, saliva, blood, or secretions — from a person’s airway. When an individual is unable to clear secretions due to a lack of consciousness or an ongoing medical procedure, suction machines help them breathe by maintaining a clear airway.
In practice, care professionals use suction machines as an integral part of a treatment plan when a patient’s airway is partially or completely obstructed. Some common uses include:
- Removing respiratory secretions when the patient is unable to
- Assisting a patient that is vomiting while seizing or unconscious
- Clearing blood from the airway
- Removing a foreign substance from a patient’s windpipe and/or lungs (pulmonary aspiration)
Since they can be used in conjunction with other medical technologies to treat a variety of life-threatening conditions, aspirators have become a mainstay in both pre-hospital and in-hospital settings. Given their ubiquity, it’s common to have questions about their uses and functions.
Common Uses for Suction Machines
Suction machines are often used when a patient is experiencing liquid or semi-solid blockages in their pharynx, trachea, or other oral cavities. However, the ideal suction device may vary depending on a patient’s condition. Here are a few scenarios where patients or professionals may use a portable suction machine.
Ongoing Patient Care
Patients may require portable suction machines in their home if they are unable to clear their own secretions for a variety of reasons. This includes patients who are receiving palliative care and find it difficult or impossible to clear their own secretions, individuals with chronic illnesses (COPD, ALS, cystic fibrosis, bronchiectasis, etc.), or patients who have undergone a tracheostomy.
Pre-hospital
Portable aspirators are very common in a pre-hospital setting, as they play a crucial role in helping emergency responders establish ABC (airway, breathing, and circulation). In practice, pre-hospital providers often use portable suction machines to treat a variety of patients. This includes trauma victims with blood in their airway, overdose victims with vomit in their airway, and other victims that are experiencing a respiratory emergency.
In-Hospital
Most hospitals have rooms that are outfitted with stationary, wall-mounted suction machines. Care teams often use stationary aspirators as a part of standard procedures such as tracheostomies, sinus-related ailments, and tonsillectomies.
However, hospitals often have a few portable devices for certain use cases. For example, if a patient needs an aspirator but there is no wall-mounted aspirator in the patient’s room, the care team will locate and retrieve a portable aspirator instead of moving the patient to another room. Additionally, they’re used to treat patients outside of a room when hospitals are at capacity.
Benefits of the solution
Today, several types of suction devices are available for use or rent by both hospitals and patients.
- Manual suction devices —Manual devices do not use electricity, and their design can be as simple as a handheld bulb that’s used to expel mucus from a child’s nasal cavity. They’re often used in emergency settings since they don’t require electricity to function and are usually small and portable. However, it is difficult to use manual suction devices consistently and effectively over a long period of time.
- Stationary suction machines —For decades, stationary devices were the most common machines, as they were reliable, effective, and consistent. However, their lack of portability left a lot to be desired. Patients couldn’t be treated with a stationary suction machine during transport and it could only provide emergency care within a hospital’s four walls.
- Portable suction machines —Portable suction machines are growing in popularity due to advances in aspirator and battery technology. Portable aspirators are designed to be lightweight and easy to move or transport, making them perfect for both patients and medical professionals.
Manual, stationary, and portable suction machines all have their place in a modern care environment. Each has its own set of strengths, and medical professionals may utilize multiple types of suction machines during different phases of treatment.
Skills requirements (to use the solutions by healthcare and social care employees)
Before using a suction machine, make sure you have received appropriate training for the device.
Examples of companies producing the tool
Smec
Omnia Health
DIGITAL SOLUTIONS FOR HEALTH CARE
Autism Spectrum Test
Rationale (4 line justifying the need of using the solution)
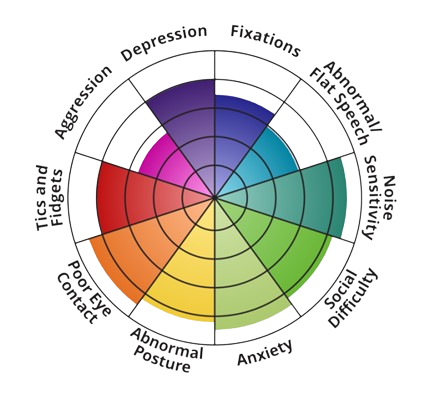
The Autism-Spectrum Quotient Test (abbreviated to AQ) is a diagnostic questionnaire designed to measure the expression of Autism-Spectrum traits in an individual, by his or her own subjective self-assessment. The Autism Spectrum Test is based on a famous and well-regarded inventory for the assessment of the clinical concept of autism spectrum disorders, which is regarded as a range of interlinked neurodevelopmental disorders. The 10 dimensions measured by this test are: Depression, Fixations, Abnormal/Flat Speech, Noise Sensitivity, Social Difficulty, Anxiety, Abnormal Posture, Poor Eye Contact, Tics and Fidgets, and finally Aggression. A definitive mental health assessment can be made only by a qualified mental health professional.
Features of the solution (how the solution works)
The AQ was designed for adults with average IQ or above, who comprise at least 50% of the autism spectrum. Individuals are instructed to respond to each of the 50 items with one of four responses: ‘definitely agree’, ‘slightly agree’, ‘slightly disagree’, and ‘definitely disagree’. Responses are scored using a binary system, where an endorsement of the autistic trait (either mildly or strongly) is scored as a +1, while the opposite response is scored as a 0, leading to a maximum score on the AQ of 50. An alternative scoring system has also been employed that uses a 4-point Likert scale. AQ items are counterbalanced to avoid a response bias, so that half of the ‘agree’ responses and half of the ‘disagree’ responses endorse the autistic trait. The AQ includes questions about both ability and preference. The questionnaire is not suitable for individuals with low IQ, low verbal ability, or language impairment, as it relies on receptive understanding of the 50 questions.
It is called a spectrum because in all of the areas shown on this color wheel, every autistic person has a different level of deficit or ability. This means that every individual with autism has a one-of-a-kind experience and is uniquely located somewhere on the spectrum. The autism spectrum encompasses a range of neurodevelopmental conditions, all pointing to the presence of disorders such as classic autism, Asperger’s syndrome, or Rett’s syndrome. However, there is considerable variation in the type and severity of the symptoms.
Benefits of the solution
This test combines the insights of several prior efforts to research the autism spectrum to bring you a single, composite test measuring autism spectrum occurrences across 10 different domains. The Autism Spectrum Quotient (AQ) Test was developed by well-known researcher Simon Baron-Cohen at the University of Cambridge in England. This test has been researched and found to be moderately accurate, even in its short 12-question version.
- Scoring range: 0–50;
- Threshold score: 26↑ (scores 26 or greater indicate you might be autistic, lower scores mean you likely are not);
- 3% of autistic people score 32 or higher
- Most non-autistic males score17 on average
- Most non-autistic females score 15 on average
- How reliable, accurate, valid, and up to date is the test?
The AQ correctly scores autistics (both male and female) higher than neurotypicals. - Test–retest reliability (consistency of scores when a person retakes the test) was found to be good.
- Inter–rater reliability (consistency of scores when two different clinicians provide the test to the same person) was found to be good.
Research shows that the AQ is a quick tool to identify where a person is situated on the continuum from autism to neurotypicality.
The AQ doesn’t really offer much insight into specific autistic traits, as it only outputs a single score. Any scores of 26 or greater indicate the presence of autistic traits; the higher the score, the more autistic traits you have.
Furthermore, 79.3% of autistic people score 32 or higher (whereas only 2% of controls do), so scores of 32 and above are particularly significant. The AQ is particularly sensitive in distinguishing between autistic and non-autistic adult females, as 92.3% of autistic females scored 32 or higher.
Skills requirements (to use the solutions by healthcare and social care employees)
This test does not require specific skills, it can be made online also, even by the subject or by a person who suspects an unusual behavior. Basic digital skills are still required for those whi perform this test online. For the person performing the test is also necessary to have the ability to read and evaluate the data. Do note that no single test is conclusive, and not every autistic person necessarily scores above the defined threshold on each test. If you score low on the AQ but still think you could be autistic, one must try taking a few other autism tests.
After the AQ, the subject must take one of the tests below:
RAADS–R
- Identifies adults who often “escape diagnosis” due to a subclinical level presentation
CAT-Q
- Measures camouflaging, and can account for lower scores on other autism tests
Aspie Quiz
- Identifies neurodivergence and potential co-occurring conditions
Examples of companies producing the tool
The Autism Spectrum Quotient (AQ) Test was developed by well-known researcher Simon Baron-Cohen at the University of Cambridge in England and is a free resource that can be used also online on different platforms
DIGITAL SOLUTIONS FOR HEALTH CARE

Dermatoscope
Rationale (4 line justifying the need of using the solution)
A dermatoscope is a hand-held visual aid device a professional can use to examine and diagnose skin lesions and diseases, such as melanoma, Blau syndrome, Actinic prurigo, Peeling skin syndrome, Argyria, Erythropoietic protoporphyria, Lamellar ichthyosis, Harlequin ichthyosis… It can also help a professional examine the scalp, hair, and nails. Dermoscopy is a noninvasive, in vivo technique primarily used for the examination of cutaneous lesions. Dermatoscopy, epiluminescence, microscopy, incident light microscopy, and skin-surface microscopy are synonyms. Dermoscopy is performed with a handheld instrument called a dermatoscope.
Features of the solution (how the solution works)
Dermatoscopes uses light and magnification to help a dermatologist see how a person’s skin looks in more detail. Dermatoscopes help show details in the outer layer of skin that would not be visible to the naked eye. A dermatoscope functionally simulates a magnifying lens, with the added features of much higher magnification, and an adjustable inbuilt illuminating system. A hand-lens, even with in-built illumination, cannot allow visualization beyond the surface of the skin because of the reflection and scattering of light from the stratum corneum. A dermatoscope can assess structures to the depth of reticular dermis, and record images for future comparison. The basic principle of dermoscopy is transillumination of a lesion in order to study it with high magnification to visualize subtle features. Light incident on a surface like the skin may be reflected, refracted, diffracted and/or absorbed. The physical properties of the skin influence these phenomena. Most light incident on dry, scaly skin is reflected, but smooth, oily skin allows light to pass through to reach the deeper dermis. Application of a linkage or immersion fluid (like mineral oil, liquid paraffin, ultrasound gel, or 70% alcohol-based commercial solutions) over the skin, enhances translucency and improves visibility of subsurface skin structures of the lesion under investigation. The essential components of a dermatoscope include: 1) a set of achromatic lenses with magnification starting from 10× up to 200× or even higher, 2) an inbuilt illuminating system composed of halogen lamps placed within the handheld piece, and 3) a source of power supply such as rechargeable or replaceable batteries or rechargeable handles.
The newest generation of dermatoscopes includes inbuilt crossed-polarizers, which filter out scattered light from the periphery, reduce glare, and permit visualization of substratal structures without the need of a linkage fluid. Some dermatoscopes have an inbuilt photography system with supporting software for the capture and storage of images. For those dermatoscopes without inbuilt systems, special adapters are available to connect to digital cameras. Advanced devices have whole body mapping systems for detailed analysis and follow up of skin lesions over time. Newer handheld units can attach to smart-phones for easier image capture and documentation.
Dermatoscopes may be with or without an in-built image capturing facilities. A simple hand-held dermatoscope looks like a broader version of an otoscope and lacks an inbuilt camera. Image-capture dermatoscopes have a special lens, which mounts onto a conventional or a digital camera. United serial bus (USB) video-dermatoscopes have a high-resolution camera fitted to the handpiece that allows visualization of the image on the computer screen as well as capturing videos. Advanced dermatoscopes have an analytical capability in addition to image-capture.
Dermoscopy is performable by either the non-contact or the contact technique. In the contact technique, the glass plate of the instrument touches the lesion through the linkage fluid. In the non-contact technique, the cross-polarized lens absorbs all the scattered light and hence allows only light in a single plane to pass through it without contact of the lens with the skin. The contact technique gives better illumination and resolution. The advantage of the non-contact technique is the prevention of inter-patient infections. Avoidance of cross-infection in the case of contact dermoscopy is by using a barrier like a cling film or adhesive tape over the lesional skin.
Although the advent of high-quality dermatoscopes with polarizers has rendered the use of linkage fluids and contact dermoscopy almost redundant; it is worthwhile to be cognizant of the concept. The linkage fluid enhances the translucency of stratum corneum facilitating imaging of deeper structures. Many substances can function in this capacity including mineral oil, ethanol, liquid paraffin, and ECG/USG gel. The latter remains the most commonly used linkage fluid in the current era, especially for onychoscopy.
The recent improvements in the manufacturing of dermatoscopes include – reduction in dimensions and bulk of the device, wi-fi connectivity for USB dermatoscopes, digital image analysis, and attempts to incorporate artificial intelligence to create an automated diagnostic unit.
Benefits of the solution
The dermascope allows the visualization of subsurface skin structures not visible to the naked eye. The dermoscopic images may be photographed or recorded digitally for storage or sequential monitoring for change. It can help identify lesions and differentiate melanocytic lesions from dysplastic lesions, melanomas, or non-melanoma skin cancers such as basal cell carcinoma or squamous cell carcinoma. Furthermore, over the past several years, the use of dermoscopy has expanded to include utilization for diagnosis of dermatological disorders including inflammatory dermatosis, pigmentary dermatosis, infectious dermatosis, and disorders of the hair, scalp, and nails. As the utility of dermoscopy continues to expand, practitioners in almost all specialties should be familiar with this simple, non-invasive and high-yield diagnostic technique. This activity reviews the various uses for dermoscopy across multiple specialties and stresses the role of team-based interprofessional care.
The usage of a dermascope may result in confirmation of clinical diagnosis, often avoiding the need for a skin biopsy. Although a skin biopsy and clinicopathological correlation (CPC) remain the gold standard for cutaneous diagnosis, dermoscopy often helps tilt the clinical differential in instances where it identifies a distinct pattern. Its use has been most popular for differentiation between melanocytic nevi and melanomas. However, the indications of dermoscopy are continually expanding and include an evaluation of hair disorders, general pigmentary disorders, appendageal tumors, inflammatory disorders like psoriasis and lichen planus, and for pre- and post-evaluation of therapeutic procedures. In the current scheme of things, we are gradually moving from CPC to clinico-dermoscopic-pathological correlation (CDPC).
Skills requirements (to use the solutions by healthcare and social care employees)
Dermoscopy is not only for dermatologists, rather the skill should be acquired and customized by other specialists too, especially general practitioners/family physicians, pediatricians, and dermatosurgeons. Pediatricians in particular must get acquainted with dermoscopy as the non-invasive and visually engaging property of dermoscopy and its images make paediatricians’ interaction with an anxious child much more convenient.
The use of dermoscopy by general physicians is very low. The impact of subspecialisation and dermatoscopy use have a big impact on the accuracy of melanoma diagnosis among primary care doctors worldwide. Regrettably, many barriers have resulted in extremely low usage of dermoscopy by general/family physicians. Some of these barriers include – costs of dermoscopy—both the equipment cost and the relatively inadequate reimbursement for its use in practice, the need for dermoscopy training, lack of information about learning resources and the unwillingness to invest time, both for training and to use dermoscopy in practice.
In order to use a dermascope a professional must acquire specific imagery skills, beside the basic knowledge about how to use a computer/laptop, basic knowledge about internet connection and a basic level of technology proficiency.
Examples of companies producing the tool
Bomtech, Dermlight, Dermoscan, Heine, Luxamed, Opticlar Vision, Italeco
DIGITAL SOLUTIONS FOR HEALTH CARE

Mobile applications for sleep disorder
Rationale
Due to the modern lifestyle and work conditions, characterized by anxiety and stress, sleeping problems are becoming more common all over the world. Rapid progress in digital technology has led to the development of fully automated digital programmes that can facilitate the sleeping process and quality, allowing for improved productivity and better overall quality of physical and mental life.
Features of the solution
Mobile sleep interventions utilize cognitive behavioral therapy (CBT) for insomnia in order to identify what works to improve people’s sleep. These interventions incorporate proven techniques that have been developed over decades of research.
Initially, the user enters data to the application regarding his sleep needs and problems, as well as information that could be affecting his/her sleep (i.e. age, gender, working hours, medication, caffeine intake). Then, a toolkit is fitted out to these needs, with tools and techniques to address sleep issues.
Users can set goals based on what they want to improve, test their sleep through specialized in-depth questionnaires and build their personal program based on their set goals. Also, the intervention can make suggestions for the improvement of the user’s environment and habits.
In this context, a person can learn how to address the factors that impact their sleep, such as lifestyle or occupation and practice cognitive techniques in order to manage their thoughts and stress.
The intervention does not automatically measure sleep duration, for example through a connected smart watch, but the user keeps a sleep diary to log his/her sleep duration and frequency of waking up during that time. Mobile sleep interventions are available through the respective app stores of mobile devices.
Benefits of the solution
Evidence from clinical trials for the management of insomnia have shown that such interventions can lead to significant improvement in insomnia.
Some of the recorded benefits:
- Significant reduction in time to fall asleep;
- Fewer awakenings during the night;
- Boost in daytime energy and concentration;
- Feeling more energetic throughout the day;
- Enhanced mood and productivity;
- Drug-free: this solution impacts the sleep naturally without pills or potions;
Additionally, healthcare professionals (especially sleep experts) can benefit from such solutions, since their workload is expected to be reduced, as patients can manage their condition mainly on their own through the solution and, thus, require less physician visits.
Skills requirements
The ability to use smart mobile devices (phone, tablet) is necessary for the users. Also, users must be able to use the solution with care regarding data privacy.
Introductory video
Examples of companies producing the tool
https://www.sleepio.com/
DIGITAL SOLUTIONS FOR HEALTH CARE

Nebulizer Care Appliance
Rationale (4 line justifying the need of using the solution)
A nebulizer is a small machine that turns liquid medicine into a mist. You sit with the machine and breathe in through a connected mouthpiece. Medicine goes into your lungs as you take slow, deep breaths for 10 to 15 minutes. The main advantage of nebulized drugs is that they are deposited directly into the respiratory tract and thus higher drug concentrations can be achieved in the bronchial tree and pulmonary bed with fewer adverse effects than when the systemic route is used. Breathing the medication straight into the lungs works better and faster than taking the medication by mouth.
Features of the solution (how the solution works)
A nebulizer changes medication from a liquid to a mist so you can inhale it into your lungs.
Nebulizers come in home (tabletop) and portable models. Home nebulizers are larger, and you have to plug them into an electrical outlet. Portable nebulizers run on batteries, or you can plug them into a car outlet. Some are only a bit bigger than a deck of cards, so you can carry them in a bag or briefcase.
You may need a doctor’s prescription for a nebulizer, or you can get one at your pediatrician’s office. Many people also get breathing treatments at their doctor’s office.
How to use a nebulizer
- Wash your hands.
- Connect the hose to an air compressor.
- Fill the medicine cup with your medicine.
- Attach the hose and mouthpiece to the medicine cup.
- Place the mouthpiece in your mouth.
- Breathe through your mouth until all the medicine is used.
- Turn off the machine when done.
- Wash the medicine cup and mouthpiece with water and air dry until your next treatment.
Benefits of the solution
The main advantage of nebulized drugs is that they are deposited directly into the respiratory tract and thus higher drug concentrations can be achieved in the bronchial tree and pulmonary bed with fewer adverse effects than when the systemic route is used. Breathing the medication straight into the lungs works better and faster than taking the medication by mouth.
Skills requirements (to use the solutions by healthcare and social care employees)
A nebulizer doesn’t require special skills or training, the instruction manual is enough resource to assemble the equipment. The medicine that must be administrated has a receipt written by a doctor.
Examples of companies producing the tool
Omron, Philips, Viatom, Promed
DIGITAL SOLUTIONS FOR HEALTH CARE

Polysomnograph with EEG
Rationale ( 4 line justifying the need of using the solution)
Polysomnograph can be used to perform a comprehensive overnight PSG study at a patient’s home and in an ordinary hospital room. With this tool, there is no need to arrange a sleep lab and the medical personnel continuously monitoring the exam progress is no longer required. Ambulatory PSG is not less effective than clinical PSG, but in addition, is more comfortable and cost-benefit for a medical facility.
Features of the solution (how the solution works)
Sleep disorders, particularly breathing-related sleep disorders, are significant health problems that require polysomnography (PSG) for accurate diagnosis and treatment. PSG comprises overnight neuro-cardio-pulmonary monitoring. The term polysomnography refers to the simultaneous recording of multiple sleep parameters, including a limited electroencephalogram, respiratory parameters, chest excursion, limb movements, and the electrocardiogram. Polysomnography is important for assessing a variety of sleep disturbances, including disorders such as sleep-related breathing disorders (including obstructive sleep apnea), rapid eye movement behavior disorder, and periodic movements of sleep. The multiple sleep latency test and maintenance of wakefulness test are studies that are especially useful in the evaluation of narcolepsy and other hypersomnia.
A sleep disorder generally occurs for one of two reasons. It may represent a primary disorder of a mechanism controlling sleep or failure of a specific end organ, such as the upper airways and lungs. As in all of clinical medicine, testing must be ordered and interpreted within the context of the patient’s clinical presentation, with a clear understanding of the questions to be answered and the inherent limitations of the study proposed. Most patients present with complaints of excessive daytime sleepiness, difficulty initiating or maintaining sleep, or some sort of unpleasant event that occurs during sleep. Detailed medical and sleep histories with careful attention to underlying medical and psychiatric illness, daytime schedules, lifestyle issues, medications, and drug use are prerequisites for the intelligent analysis of the problem and planning of the appropriate testing. A complete physical examination should always be obtained before referral for study. Sleep logs, which document daily sleep–wake behaviors, may be valuable tools that complement both the office history and the interpretation of the objective data acquired in the sleep laboratory.
Various portable ventilators are available, driven by demands for equipment suitable for different clinical situations and environments. Their design reflects availability of gas and electrical supplies and the modes of ventilatory support required by the patient population. When transporting critical care patients, provision for estimated gas and electrical requirements should be made. A ventilatory mode suited to the patient’s clinical condition should be selected and trialed before departure. An appreciation of how different portable ventilators function, preferably supported by comparative data, can help when an organization purchases such equipment. Understanding the strengths and weaknesses of a specific ventilator and breathing circuit may help anticipate and prevent complications during transfer.
Benefits of the solution
The polysomnograph is a very useful tool to be used in testing and diagnose sleep-related breathing disorder. The use of polysomnograph has several clinic applications:
- Suspicion of sleep-related breathing disorders.
- Treatment and follow up of sleep-related breathing disorders.
- In combination with the MSLT for suspected narcolepsy.
- Evaluation of sleep-related behaviors that are violent, potentially injurious, or do not respond to conventional therapy.
- To assist in the diagnosis of paroxysmal arousals that are suggestive of seizure disorder (with additional video and EEG).
- Evaluation of sleep-related movement disorders.
Even if polysomnographic analysis is not specifically required in the assessment of a sleep complaint, clinicians often find that the judicious use of polysomnography may be remarkably revealing. For example, although the diagnoses of the various insomnias do not include the requirement of a PSG, polysomnographic study may reveal subtle sleep-disordered breathing, leg movements inducing arousal, or show that no objective impairment of sleep correlates with the patient’s subjective report.
Skills requirements (to use the solutions by healthcare and social care employees)
The monitoring of sleep and the interpretation of sleep study findings are complex and require a distinct skill set including a detailed knowledge of physiological changes during sleep, electroencephalography (EEG), respiratory monitoring, and electrocardiography (ECG).
Polysomnographic interpretation requires both an independent analysis of the component measurements and an overall synthesis of how these variables interact with each other. Most reports include a quantitative report of sleep architecture, respiratory measures, EKG, limb movements, and a limited description of EEG. Diagnostic requirements for specific disorders using these measures are described in Tables 7 to 11. Qualitative interpretation of the PSG is also important, and relies on the polysomnographer’s ability to identify patterns of interaction between variables that vary from the norm and may be disease specific. A summary of statistics does not replace an epoch-by-epoch review of the record. Interpretation is dependent on the clinical context, making it important that the clinician approaches the process of reading a sleep study with an understanding of the patient’s medical background and the specific questions posed
Examples of companies producing the tool
Allengers, Neurosoft, Deymed Diagnostic
DIGITAL SOLUTIONS FOR HEALTH CARE

Portable ventilators
Rationale (4 line justifying the need of using the solution)
Portable ventilators are durable, portable tools, designed to provide critical ventilation support during mass casualty events. Portable ventilators are commonly battery-powered, and some models can run on multiple power sources. The tool is needed during critical care transportation, at home when lung diseases result in respiratory insufficiency (patients may receive support nocturnally or continuously, provided invasively by tracheostomy or non-invasively by facemask) in case of aeromedical evacuation etc.
Features of the solution (how the solution works)
Ideally, a portable ventilator, including oxygen and battery supplies, should be lightweight, robust, and able to function in demanding environments with little maintenance. It must use available gas or electrical supplies sparingly. It should be inexpensive, simple to operate, and provide a range of effective ventilatory modes.
Sufficient oxygen is required to meet the patient’s requirements. It may also be used to provide a background rate of gas flow (bias flow) through the breathing circuit, or to control the ventilator cycle itself. During critical care transportation, oxygen is commonly supplied from gas cylinders. Oxygen concentrators can be used if supplying cylinders is problematic, such as in a military field hospital. For aeromedical evacuation, low-pressure liquid oxygen systems can provide three times more gaseous oxygen than a similar sized cylinder.
Domiciliary ventilation is associated with survival benefits in patients with neuromuscular disease and has also been used when chest wall and lung diseases result in respiratory insufficiency. Patients may receive support nocturnally or continuously, provided invasively by tracheostomy or non-invasively by facemask. The LTV series of ventilators was originally developed for domiciliary ventilation. Supplemental oxygen is usually not required in patients with neuromuscular disease and the ability of these ventilators to operate on battery without compressed gas supply maximizes portability, enabling them to be mounted on electrical wheelchairs. The emergence of non-invasive ventilation without tracheal intubation has inevitably resulted in the requirement to transfer patients undergoing this therapy. Gas leakage from around the mask is often a problem within the critical care environment and slight dislodgement during transport may increase leak and significantly reduce effectiveness. The combination of sophisticated sensors and basal gas flows within the patient circuit allows microprocessor-controlled ventilators to compensate for circuit leaks. There is increasing experience in the use of these ventilators for noninvasive ventilation during the transfer of acutely unwell patients, and domiciliary ventilation in chronic disease. Remember that expiration will still occur through the patient circuit exhalation valve so a non-vented mask is required.
Benefits of the solution
Various portable ventilators are available, driven by demands for equipment suitable for different clinical situations and environments. Their design reflects availability of gas and electrical supplies and the modes of ventilatory support required by the patient population. When transporting critical care patients, provision for estimated gas and electrical requirements should be made. A ventilatory mode suited to the patient’s clinical condition should be selected and trialled before departure. An appreciation of how different portable ventilators function, preferably supported by comparative data, can help when an organization purchases such equipment. Understanding the strengths and weaknesses of a specific ventilator and breathing circuit may help anticipate and prevent complications during transfer.
Skills requirements (to use the solutions by healthcare and social care employees)
Each application entails differences in the clinical condition of patients, operator experience, and demands of the environment. A single device is unlikely to be ideal for all situations; therefore, a range of ventilators are available. A previous preparation is necessary before recommending a certain ventilator and also basic digital skills such as analyzing data and knowledge of use of digital devices.
Examples of companies producing the tool
Oxivent, Philips, Oxymag
DIGITAL SOLUTIONS FOR HEALTH CARE

Universal Heart Simulator
Rationale (4 line justifying the need of using the solution)
The universal heart stimulation (UHS) is a portable electronic device that automatically diagnoses the life-threatening cardiac arrhythmias of ventricular fibrillation (VF) and pulseless ventricular tachycardia, and is able to treat them through defibrillation, the application of electricity which stops the arrhythmia, allowing the heart to re-establish an effective rhythm. UHS mode functions as a diagnostic tool in EP examinations, particularly in clinical protocols for the induction of supra-ventricular tachycardia
Features of the solution (how the solution works)
An electrical stimulus is generated by the sinus node (also called the sinoatrial node, or SA node). This is a small mass of specialized tissue located in the right upper chamber (atria) of the heart. The sinus node generates an electrical stimulus regularly, 60 to 100 times per minute under normal conditions. The atria are then activated. The electrical stimulus travels down through the conduction pathways and causes the heart’s ventricles to contract and pump out blood. The 2 upper chambers of the heart (atria) are stimulated first and contract for a short period of time before the 2 lower chambers of the heart (ventricles).
The electrical impulse travels from the sinus node to the atrioventricular node (also called AV node). There, impulses are slowed down for a very short period, then continue down the conduction pathway via the bundle of His into the ventricles. The bundle of His divides into right and left pathways, called bundle branches, to stimulate the right and left ventricles.
The stimulation impulse generates an electrical field, which causes a decrease in the baseline membrane potential (hypopolarisation) by an ionic current. As a consequence, further sodium channels are opened until the threshold potential is reached and the depolarisation of the cell is initiated. The minimal amount of energy required for this process is called stimulation threshold, which depends on the electrode surface, the stimulation impedance, the alignment of the myocardial fibers in the electrical field, the distance to excitable tissue and the polarization current. The relationship between pacing current and impulse duration is described by rheobase and chronaxy. Implantable pacemaker devices work with biphasic stimulation impulses, which allow a recharge of the delivered impulse energy from the heart to the stimulator and therefore avoid an electrolysis.
Benefits of the solution
Physicians are offered an ideal combination of touch screen and hard key controls as well as personalized protocols. Intuitive menus anticipate physicians’ needs, making it as easy as possible to stimulate the heart.
Even in a pandemic, programs like cardiac rehabilitation are an important component in getting people back to the life they wish to lead.
The improved understanding of the basic principles of cardiac pacing led to the development of modern stimulation electrodes. Steroid eluting leads avoid an increase in pacing threshold in the initial period. The geometrical surface of electrodes was reduced with the effect of lower pacing thresholds. The introduction of new electrodes with a porous or fractal surface led to a reduction in polarisation and therefore to an improved stimulation with regard to energy delivery. The new pacemaker generation allows a monitoring or analysis of stimulation. With the help of certain algorithms the efficacy of every single ventricular stimulus is monitored (autocapture function) and the pacing amplitude automatically adjusted to the actual situation. This prolongs the pacemaker’s life and simplifies follow-up.
Skills requirements (to use the solutions by healthcare and social care employees)
When programming the pulse generator at implantation, the clinician must also consider the acute to chronic evolution of the stimulation threshold. Because an acute rise in threshold typically occurs during the first several weeks after lead implantation, voltage and pulse duration may need to be programmed to higher values than needed for chronic pacing. The physician should reevaluate the stimulation threshold after the acute rise (and sometimes subsequent fall). For most patients, the pacing system can be programmed to chronic output settings at a follow-up evaluation about 6 weeks after lead implantation. Although these recommendations may not be as applicable to patients receiving a steroid-eluting lead, caution is still warranted.
- Use of stethoscope:
A real stethoscope can be used - Heart Sounds and Murmurs
Auscultation in relation to synchronized electrocardiograms and findings.
-differentiation of S1, S2, S3 and S4
-discrimination between systolic and diastolic murmurs - Palpation of arterial pulse at 8 sites:
Slight variations of the arterial pulse waves under different cardiac conditions or arrhythmias can be detected by palpation - Observation of jugular vein pulses:
The strength and timing of “α “and “V” waves vary with cases - Palpation of Cardiac Impulses:
RV, LV and DLV are simulated and can be palpated - Real time dynamic charts on the screen:
-phonocardiogram
-sphygmogram (CAP/JVP/AC)
-electrocardiogram (ECG) - Respiratory Sounds and Abdominal Movement:
Respiratory cycle is represented to understand respiratory related phenomena
Examples of companies producing the tool
Biotronik
DIGITAL SOLUTIONS FOR HEALTH CARE

Urine analyzer
Rationale (4 line justifying the need of using the solution)
A urine analyzer is a device used in the clinical setting to perform automatic urine testing. The units can detect and quantify a number of analytes including bilirubin, protein, glucose and red blood cells.
Features of the solution (how the solution works)
The essence of the test principle of the urine analyzer is the absorption and reflection of light. The liquid sample is directly added to the multi-linked reagent strip with different solidified reagents. The corresponding chemical composition in the urine causes the color of the module containing various special reagents on the multi-linked reagent strip to change. The color depth is consistent with the specific chemistry in the urine sample. The component concentration is proportional; the multi-link test strip is placed in the colorimetric injection tank of the urine analyzer, and each module is irradiated by the light source of the instrument and produces different reflected light. The instrument receives the light signal of different intensity and converts it into the corresponding The electrical signal is calculated by the microprocessor (CPU) to calculate the reflectance of each test item, and then compared with the standard curve and corrected to the measured value, and finally the result is automatically printed out in a qualitative or semi-quantitative manner.
This type of instrument is generally controlled by a computer, and the color change on the test strip is measured semi-quantitatively by using a spherical area spectrometer to receive dual-wavelength reflected light. There are several reagent pads containing various reagents on the reagent strip, each of which reacts independently with the corresponding components in the urine, and displays different colors. The depth of the color is proportional to a certain component in the urine. There is another one in the reagent strip. “Compensation pad”, as the background color of urine, compensates for errors caused by colored urine and instrument changes.
The instrument usually calculates the reflectance automatically according to the following formula, and then compares with the standard curve, and automatically finds the corresponding results of various components. If the content of a certain component in urine is high, the reflection light of the corresponding reagent pad is darker, otherwise it is strong .
Benefits of the solution
Automated urine analyzers aids in precise and accurate urine results while reducing turnaround time and workload of a laboratory. The results also guide the clinical towards a probable diagnosis and empirical treatment could be initiated at the earnest.
A urinalysis is a test of one’s urine. It’s used to detect and manage a wide range of disorders, such as urinary tract infections, kidney disease and diabetes. A urinalysis involves checking the appearance, concentration and content of urine.
Automated urinalysis offers the benefits of convenience, efficiency, and increased sensitivity for detecting renal and urinary tract abnormalities. The true value may lie in the ability to efficiently screen and report out urine samples that lack pathologic findings. In our experience at a large clinical lab, up to 70% of urine samples can thus be screened and reported without the need for a confirmatory manual microscopy, saving a considerable amount of time and labor. All of the automated sediment analyzers reviewed have comparable performance characteristics with improved standardization over manual microscopy. The system a lab chooses can be based on individual preference for the advantages each has to offer.
What can be found in urine test?
- Acidity, or pH. If the acid is abnormal, one could have kidney stones, a urinary tract infection (UTI), or another condition;
- This can be a sign one’s kidneys aren’t working right;
- Glucose;
- White blood cells;
- Nitrites;
- Bilirubin;
- Blood in the urine.
Skills requirements (to use the solutions by healthcare and social care employees)
A urinalysis analyzer, that will evaluate the urine and provide a printout of the results, known as Point of Care Testing must not use unless you have received specific training for doing so.
Examples of companies producing the tool
ACON Laboratoires, Cardinal Health
DIGITAL SOLUTIONS FOR HEALTH CARE

Vascular Medical Dopplers & Displays
Rationale (4 line justifying the need of using the solution)
A Vascular Doppler is a medical diagnostic test used to quickly review the body’s circulatory system to identify irregularities and concerns with blood flow in large arteries and veins. A Vascular Doppler units perform a range of very valuable vascular assessments to help diagnose vascular diseases and life-threatening conditions.
Features of the solution (how the solution works)
A Vascular Doppler is a medical diagnostic test used to review the body’s circulatory system to identify irregularities and concerns with blood flow in large arteries and veins. A Vascular Doppler units perform a range of very valuable vascular assessments to help diagnose vascular diseases and life-threatening conditions. Vascular assessments are critical to evaluate the health of the vascular system and to help prevent serious cardiac events.
Vascular Doppler ultrasound is a non-invasive diagnostic test used to determine the amount of blood flow moving through blood vessels by aiming high-frequency sound waves (ultrasound) at red blood cells and then receiving them back via the traducer/probe to measure for strength and frequency. There is an auditory and visual display to record the sounds and display pictures. Most ultrasound machines today have Doppler capabilities to measure blood flow and to evaluate veins and arteries in the organs that the ultrasound is visualizing. This is called Duplex ultrasound. Color images can be superimposed on the vessels to see which way the blood is flowing.
The Doppler ultrasound is named for Christian Doppler, a 19th-century physicist who discovered a way to measure sound waves reflected from moving objects. This is known as the Doppler effect.
The ultrasound probe sends sound waves into your body. The sound waves bounce off of moving blood cells in blood vessels and go back to the probe to be detected. The computer looks at the change in pitch (low or high sounds) between the sound waves sent into your body and the echo (sound that bounced back) to figure out the direction of blood flow and how fast the blood is moving.
This information provides information about:
- Your circulation, such as how fast or slow blood is moving.
- If something is stopping blood flow.
- Blood going in the wrong direction or pooling in a blood vessel.
Depending on the reason for the test, you may lie on your back or side on an exam table, or you may sit up.
During the test:
- The sonographer applies a small amount of gel to your skin. The gel helps the sonographer glide a small probe over the skin. It also helps sound waves travel.
- The transducer sends painless sound waves through your skin into your body. The sound waves are high frequency and you won’t hear them.
- The sound waves reflect off the moving blood cells, causing the pitch of the sound waves to change. You may hear a whooshing sound from the ultrasound machine.
- The transducer detects changes in the sound wave.
- A machine records the sound wave changes and converts them into images or graphs for your provider to review.
- The sonographer cleans the gel from your skin at the end of the test.
Benefits of the solution
Vascular assessments are critical to evaluate the health of the vascular system and to help prevent serious cardiac events.
A Doppler ultrasound may help o quicker diagnose many conditions, including: blood clots, poorly functioning valves in your leg veins, which can cause blood or other fluids to pool in your legs (venous insufficiency) Heart valve defects and congenital heart disease.
Skills requirements (to use the solutions by healthcare and social care employees)
A sonographer, a specialist in ultrasound imaging technology, performs this test. The test may take 30 to 60 minutes. The use of the tool requires basic skills as analyzing data and knowledge of use of digital devices
Examples of companies producing the tool
Philips, Siemens